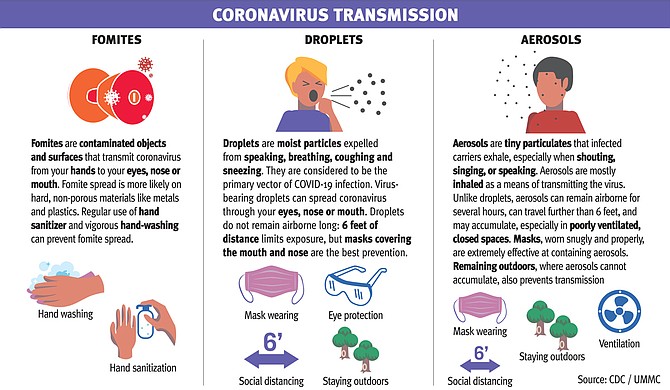
The most up-to-date information on COVID-19 confirms many of the baseline infection-control standards—like masks and social distancing—but also reveals a more complete understanding of what makes the virus dangerous. Photo courtesy CDC/UMMC
After months of COVID-19 growth, Mississippi is in the middle of a stable decline in viral spread, lessening the stress placed on the health-care system and reducing the deaths that follow every new cluster of cases. By Wednesday, Sept. 9, the seven-day rolling average of new cases had dropped to 491, the first time that number had declined below 500 since June 21, 2020.
State health leadership attributes the drop in transmission to widespread acceptance of the same principles of infection control known to protect public health at the peak of the pandemic in Mississippi.
But success can be fleeting in the fight against coronavirus.
While Mississippi's numbers are on a markedly positive trend, the state is now mostly open, with students in schools and colleges and many businesses back to work on premises. The close proximity provides the tinder for the rampant spread of the virus if the measures are abandoned.
State Health Officer Dr. Thomas Dobbs highlighted on Sept. 10 the progress being made with the help of masking and social distancing. "We can see that our efforts have been fruitful, even in context of outbreaks in college towns, (and) transmission in K-12, which has really gone better than we anticipated," he said.
In the first month of full in-person classes, which have become the norm for the 2020 fall semester in Mississippi, more than 17,000 students, teachers and staff members have been reported quarantined as a result of exposure to COVID-19. At least 1,700 have tested positive, though the Mississippi State Department of Health's contact-tracing efforts have shown that it is large-scale social gatherings, like block parties and sorority and fraternity life events, that have led to the most dramatic amounts of transmission around schools.
With months of research, testing and tracing to draw from, the Jackson Free Press reached out to experts including Dr. Bhagyashri Navalkele, medical director of infection prevention and control at the University of Mississippi Medical Center in Jackson as well as state health leadership from MSDH, to provide an update on COVID-19 prevention and control standards and where they now stand.
Detecting Coronavirus
Coronavirus disease often outwardly presents as a respiratory ailment similar to the flu, with common symptoms of coughing, sore throats, nasal congestion, muscle fatigue and shortness of breath. A valuable early-warning sign of COVID-19 for even mild, but still highly infectious, cases is a loss of smell or taste. Experiencing this symptom in particular is a critical warning sign that an individual likely carries coronavirus. MSDH has strenuously encouraged Mississippians to immediately quarantine and seek testing the moment they notice the absence of smell or taste.
Mississippi's testing regime has greatly improved since the early days of the virus. Individuals may seek tests at health clinics, as well as regularly scheduled mobile testing sites, a list of which is at healthyms.com.
But asymptomatic transmission—meaning contracting the disease from exposure to a person displaying absolutely no symptoms—is absolutely possible.
The CDC has confirmed the presence of asymptomatic carriers among school- children, long-term care facility residents, and others, as well as asymptomatic transmission of the virus. This means that testing and quarantining of individuals exposed to known cases is critical; preventing only symptomatic transmission cannot prevent the virus from spreading.
Fomites, Aerosols, Droplets
One of the ongoing debates in the world's growing understanding of coronavirus is the method of transmission: how the virus travels from host to host.
There are three primary vectors behind the spread of coronavirus, and medical experts are increasingly certain that all three play some role in the pandemic.
A fomite is an inanimate object which has become contaminated with viral particles. Virtually anything can become a fomite, and thus transmit coronavirus, but current research suggests that hard, non-porous surfaces, such as plastic and stainless steel, are more likely to retain a potentially infectious reservoir of the virus for an extended period of time.
Droplets are, as one might expect, small, moist particles that contain infectious viral contaminants. Droplets are most easily spread through coughing and sneezing, although talking, singing and breathing are also capable of spreading droplets up to 6 feet away.
The present consensus on COVID-19 holds droplet transmission to be the single largest source of new infections.
"Most of the data we have so far still suggests that droplet transmission is the most common mode of transmission for the virus," Navalkele said.
An aerosol is a light, extremely tiny particle that emerges from the lungs when an individual exhales. Aerosols travel much further than droplets. When one hears the term "airborne" transmission in the context of coronavirus, aerosols are the culprit. The danger of aerosols is that they can linger in the air longer and farther than the heavier droplets, which can only remain in the air for a matter of seconds.
This makes poorly ventilated spaces especially dangerous. Researchers have confirmed that unmasked individuals in closed spaces without proper ventilation have spread COVID-19 to others.
Navalkele agrees that aerosol transmission is possible in tight spaces, but stressed that droplet transmission is the critical danger. "Airborne transmission is still limited to certain settings, for example, if you're sitting in a closed space," she said.
All of the various vectors that transmit coronavirus infect new hosts by traveling into their mucus membranes. This includes both the mouth and the nose, but also the eyes. Masks effectively contain both aerosols and droplets, and vigorous handwashing, supported by use of hand-sanitizer when soap is not available, is very effective at preventing fomite spread.
Dr. Jose-Luis Jimenez, a fellow of the American Association for Aerosol Research, proposed a mnemonic for preventing aerosol spread in particular: "Avoid Crowding, Indoors, low Ventilation, Close proximity, long Duration, Unmasked, Talking/singing/Yelling, (A CIViC DUTY)" Jimenez wrote in an article in Time Magazine.
Preventing Infection
The key elements of preventing transmission of COVID-19 remain, with masks critical in preventing all forms of transmission, especially in indoor settings and in large groups. Mask usage cannot decrease with cases. Relaxing mask use can even reverse a downward trend in new cases. Full adherence to correct mask usage—covering both the nose and the mouth—prevents the exhaling of droplets and aerosols, which prevents the creation of virus-transmitting fomites.
Social distancing, too, is a key part of preventing new cases of COVID-19. While masks are the most effective measure, combining them with proper social distancing means limiting the damage if masks are improperly worn or not used at all. Capacity limitations are key public-health measures to avoid a single super-spreader infecting a large mass of people, experts explain.
Because there are so many routes of infection, like the eyes, masks are not entirely effective at protecting yourself from others, experts say, but they are unmatched at protecting others from you. This is why mandates are necessary. A single unmasked individual can transmit the virus to many others who are wearing masks, especially in enclosed spaces.
"If we follow the precautions—masking, maintaining a distance of at least 6 feet, washing hands, that would reduce the risk of transmission of the virus from one person to another," Navalkele explained to the Jackson Free Press.
Viral Load
Another open question in the transmission of COVID-19 is the danger of viral load, meaning the amount of infectious particulates to which an individual is exposed. Ongoing research seeks to understand how increased exposure makes infection more likely—and how severe it makes the illness that follows.
"There's still a little bit of debate going on ... We don't completely know," Navalkele said.
Navalkele explains that an increased amount of viral exposure might cause a stronger immune response—an excessive bodily reaction that causes some of the serious organ damage known to afflict COVID-19 patients. "It is possible that if you have a higher viral load, you could have a (stronger) immune response, but it is not yet proven," she said.
As of now, MSDH considers 15 minutes of close exposure to an unmasked individual a significant risk factor, even without the presence of symptoms such as coughing or sneezing. "With symptomatic patients and asymptomatic patients," Navalkele said, "there really seems to be no difference in the viral load that they shed."
Influenza Season
Flu season in Mississippi generally occurs between November and March, and in the time of COVID-19, it presents an especially dangerous threat. The flu is not as deadly as the coronavirus at the heart of the global pandemic, but it still hospitalizes and kills many Mississippians every year.
Navalkele explained the danger of the 2020-2021 flu season as threefold.
First, the flu alone is capable of harming and killing those it infects, even children. Second, hospitalizations from flu season will crowd the state's hospitals and intensive-care units, making any future spikes in COVID-19 cases even more dangerous and burdensome. Because influenza and coronavirus share many symptoms, individuals who have the flu will present similarly to COVID-19 patients, demanding the same isolation and extra care before they are tested.
Third, Navalkele confirmed instances of individuals suffering both coronavirus and influenza at the same time, a devastating one-two punch that can easily maim or kill.
The solution is simple, according to all public-health experts contacted for this story: get a flu shot even if you usually do not. Flu shots are available at clinics, hospitals, and even many retail and pharmacy outlets. Navalkele stressed how critically important flu shots will be in reducing emergency-room visits for influenza at a time when the hospital system is already stressed.
Vaccines
As of mid-September, pharmaceutical companies and medical institutions across the globe are working on potential vaccines for COVID-19. These vaccines require large-scale testing efforts to insure their safety, split into phases, first testing their safety, then testing their large-scale efficacy. The New York Times reports that 38 vaccines are currently in some form of clinical testing.
These tests are not without their challenges. Most recently, a promising AstraZeneca trial was put on hold after a serious side effect emerged in one participant. Navalkele expressed the importance of a full testing period for any COVID-19 vaccine, and made it clear that she did not anticipate a vaccine to become globally available in 2020.
When asked if she would take a fast-tracked vaccine, Navalkele answered quickly. "I would not, until I have seen the safety and efficacy study," she said.
Email state reporter Nick Judin at nick@jacksonfreepress.com.
More like this story
- COVID-19: UMMC Expert on Emerging Knowledge of the Virus
- Expanded Voting Access Still Off Table For Mississippians
- UMMC Pandemic Expert: Social Distancing Now Will Save Lives, Lessen COVID-19 Spread
- Rules For Thee: Governor Hosts Party Hours After Signing New COVID Restrictions
- ‘An Explosive Recipe’: Delta Surge Shows No Sign Of Stopping
More stories by this author
- Vaccinations Underway As State Grapples With Logistics
- Mississippi Begins Vaccination of 75+ Population, Peaks With 3,255 New Cases of COVID-19
- Parole Reform, Pay Raises and COVID-19: 2021 Legislative Preview
- Last Week’s Record COVID-19 Admissions Challenging Mississippi Hospitals
- Lt. Gov. Hosemann Addresses Budget Cuts, Teacher Pay, and Patriotic Education




Comments
Use the comment form below to begin a discussion about this content.